

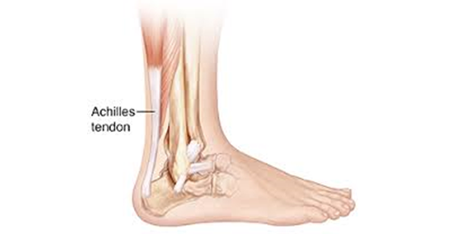
Tendo Achilles is the strongest tendon of the body. It connects the bulky Gastro-soleus muscle of calf to the posterior aspect of heel bone (calcaneum). When calf muscle contracts it pulls the heel up which helps standing on toes, walking, running and jumping. Blood supply of Tendo Achilles is limited which makes it prone for degeneration and vulnerable to injury.
Common injury and disease conditions that affects Tendo Achilles are
Acute rupture of Tendo Achilles: This injury usually happens in young individuals when foot is forcefully moved upwards at ankle and calf muscle in engaged. Commonly associated with RTA, steeping in a hole and sports related activity. Or direct injury from a sharp object. This injury is associated with contaminated local wound and exposed cut tendon.
Degenerative rupture of Achilles Tendon: This type of Tendo Achilles rupture happens due to tendon degeneration from non-insertional or insertional tendinosis and repeated loading of the tendon.
Rupture usually occurs at 6 cm from its attachment with calcaneus. There are few risk factors associated with Tendo Achilles rupture. Male ages from 30 to 40 are more prone to injury. Sports involving running, jumping, sudden starts and stops are high risk for injury. Local steroid injection around the tendon or intake of fluoroquinolone antibiotic increases rupture risk.
Chronic degenerative injuries may go unnoticeable but acute injuries are always symptomatic. Most of the time one may feel being kicked off at back of the leg, feeling a pop on snap followed by severe pain and swelling at rupture site. Inability to stand on toe tip and push off while walking. Acute injuries are very obvious on clinical examination may not need any investigation but if there is any risk factor for tendon degeneration then an ultrasound or MRI should be done to assess the integrity and health of tendon.
Both the conservative treatment with functional bracing and physical rehabilitation as well as surgical treatment by mini open apposition of tendon end with suture works well for this injury. But for open injuries operative treatment is the choice. Operative treatment in closed injuries can offer early recover and preferred over conservative for very active young and athletes. For chronic degenerative tear simple end to end suturing of tendon does not works it needs debridement and excision of the diseased portion of tendon and reconstruction of the tendon with tendon graft or transfer. Currently simple transfer of a tendon of foot muscle (responsible for big to movement toward sole) to calcaneum is gaining popularity due to its simple surgical technique and lesser complication compared to other extensive reconstruction but producing equivalent recovery.
Achilles tendinopathy:It is a condition when the affected tendon part cause pain swelling and stiffness. Its a degenerative condition of the tendon happens due to overuse, undue stress on tendon and other related risk factors. This condition affects two different part of Achilles Tendon and their presentation also different.
Non-insertional TA tendinopathy: Middle portion of Tendo Achilles has a precarious blood supply and does not heal properly from its daily wear and tear. Over the time the injuries accumulate and develop tendinopathy. There are various factors that influence microinjury to the tendon like, overuse in runner, inappropriate training method, activities involved sudden acceleration and deacceleration while running, training on hard or sloppy surface. It is also more common in individual with HTN, DM and high cholesterol. Inflammatory arthritis like ankylosing spondylitis, psoriatic arthritis also has predisposition for this condition. Fluoroquinolones antibiotic intake can increase the risk of development of tendinopathy

The main symptom is pain, swelling and stiffness. It develops gradually and usually worse at morning after weak up from sleep. Pain is worse after exercise and walking but some people may experience it in the beginning of activity also. If untreated this can lead to rupture of tendon.
Diagnosis is based on symptomatic presentation, clinical examination and assessing other risk factor. Confirmation of diagnosis and evaluation of extent of the condition can be determined by USG and MRI.
Treatment is based on symptom relief with medication, physical rehabilitation, orthotics as well as identification and modification of risk factors. Analgesic and cold compression helps in symptom reduction. Physical rehabilitation includes stretching of Achilles Tendon prevents disease progression and healing of tendon. There are various techniques have been described for optimal stretching of tendon.
If these conservative treatment does not respond there are various other non-invasive and invasive treatment is recommended.
All these are well documented treatment protocol. In advanced stage of disease debridement and resection of tendon followed by reconstruction with tendon graft or tendon transfer is required.
Insertional TA tendinopathy: It affects the tendon at its attachment with the heel bone. Repeated microtrauma of the tendon happens due to longitudinal and transverse stress near its insertion. longitudinal stress arises from tight tendon and forceful repeated activity like running, jumping and affects the superficial part. Transverse stress arises from repeated impaction of tendon with heel bone just proximal to its insertion due to its prominent tuberosity. Gradual accumulation of this injuries and impaired healing response led to insertional TA tendinopathy. Tendon attachment at heel bone get degenerative changes become thick and replaced with new bone formation at the end and within the tendon.
Common symptom is pain following activity, stiffness on rest and local tenderness. Person affected with insertional TA tendinopathy complaints off difficulty in stair climbing, walking long distance and difficulties in wearing shoe. Diagnosis is evident from symptoms and clinical examination. Imaging is required only to quantify the disease and planning treatment. X-ray is adequate but an MRI may require. But radiological description and clinical symptom may not match.

Conservative treatment consisted with pain relief with analgesic and cold compression, stretching of tendon, orthotics, modification of footwear is the main stream of treatment for insertional tendinopathy. Currently PRP is also being used for early disease and associated bursal inflammation. Surgical treatment is recommended only when a good trial of conservative treatment fails. Surgical treatment consists debridement of affected tendon after detaching from insertion, resection of bony prominence (Heglund) and bony spur following with reattachment of the tendon. Sometimes a FHL tendon transfer is required for very severe disease where a significant portion of tendon needs to be sacrificed.
Heglund Deformity and bursitis: in some individuals tuberosity part of calcaneum is very prominent and bulky leaving no space between the tendon and bone. It creates a frictional and compressive force on the tissue between the tendon and bone as well as the tendon itself. This causes reactive changes to the bursal tissue and inflammatory response develops. This condition mimics with insertional TA tendinopathy and can mislead in diagnosis.
