

Anterior knee pain refers to the pain at the front of the knee around the knee cap. Prevalence of anterior knee pain is more common in the overweight population, in adolescence and also in female gender. There is two to seven times more incidence in females than males.
Knee cap is a special type of bone that develops within the tendon of anterior thigh (quadriceps) muscle. It forms patellofemoral joint along with thigh bone (femur) and moves over the groove (trochlea) of the femur bone. The joint is stabilized by quadriceps muscle specially by its medial fibre (vastus medialis obliques), patellar tendon, medial patellofemoral ligament, retinaculum and other ligamentous bands around it. Knee cap acts as a liver for quadriceps muscle and reduces its energy requirement during knee extension and deceleration. Both are important functions for the activities like walking, running, jogging, squatting, getting up from sitting position, staircase negotiation, uphill or downhill movement.
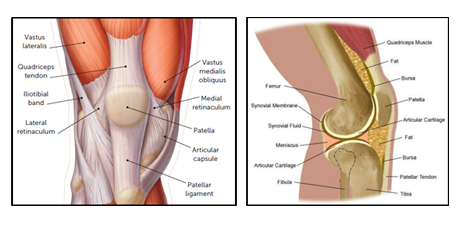
Structure of knee cap with its different attachments
There are numerous causes of anterior knee pain. It is important to identify and diagnose the exact cause of anterior knee pain for adequate treatment and prevention of further deterioration. Presentation and symptoms of few of these are very much overlapping and thus confusing. Followings are different cause of anterior knee pain
Patellofemoral Pain Syndrome
Patellofemoral pain syndrome (PFPS) is a painful condition of the knee where the pain is felt around and behind the knee cap and aggravated by at least one of the following activities like running, climbing stairs or squatting. Also complains of knee stiffness following prolonged sitting in knee flexed position. It is a common cause of knee pain in adolescents and adults younger than 60 years. It is a very common overuse stress of knee cap without any organic changes of kneecap cartilage.

Pain while getting up from squatting
Female gender and activity like running, jogging, squatting and frequent use of stairs are the established risk factors for developing patellofemoral pain syndrome (PFPS). Patellar instability plays a major role in developing PFPS. Anterior thigh muscle (quadriceps) weakness, dynamic valgus of knee where knee collapse on inner aspect from excessive valgus (outwards alignment of leg below knee) on weight bearing, foot deformities like forefoot eversion and pronation (flat foot) deformity also contribute in PFPS development. Foot deformity leads to internal rotation of the tibia and contributes to development of dynamic valgus of knee. Dynamic valgus increases lateral force on patella thus contributes to patellar mal-tracking (moves off the grove of thigh bone during knee movement). Dynamic valgus is very common in female athletes contributing to the higher incidence among them.
Diagnosis of PFPS is purely clinical. Complaining of pain during squatting is the most sensitive finding. Fluid collection in the knee joint, redness and increased temperature at knee are never associated with patellofemoral pain syndrome. Physical examination to elicit patellofemoral pain like clerk test patellar tilt test are helpful. Examination of gait, posture, foot deformity, wear pattern of footwear, quadriceps power, hamstring muscle flexibility all can give clues in finding contributory factors of PFPS development. Knee x-ray in two plane and skyline view to assess patellofemoral joint alignment is the standard basic requirement. Imaging is done for exclusion of other causes of anterior knee pain like chondromalacia patellae, trauma, infection, arthritis or other causes which were suspected clinically. Other than x-ray basic blood tests with inflammatory markers are also advised. All these test are done for exclusion of other possibilities of anterior knee pain.
Physical therapy is the one and only effective treatment solution for patellofemoral pain syndrome. Analgesics and other measures like icing are recommended for short term pain relief. Kinesio Taping of patella helps in symptomatic relief during acute phase along with analgesics. Corrective foot orthotics are recommended along with physical therapy to improve gait and kinematics of knee thus optimising the contributory factors. Knee braces do not help much and there is no role of surgical intervention. Non resolving of symptoms beyond 6-8 weeks render imaging tests like x-ray or MRI to find other cause of patellofemoral pain.

Kinesiotaping of patella
Chondromalacia patellae
It is a painful condition of the knee which arises due to softening or wear and tear of kneecap cartilage. Cartilage under the kneecap acts as a shock absorber. Overuse, injury and many other things can cause deterioration of the quality and breakdown of the cartilage. Kneecap cartilage no longer remains smooth and agile and produces pain while comes in contact with thigh bone during different activities. Symptomatic presentation of chondromalacia patellae is very much similar to patellofemoral pain syndrome. But chondromalacia patellae is associated with cartilage damage whereas patellofemoral pain syndrome is not.
It affects young adults especially females more than any other age group. Common among runners, joggers, skiers, soccer players, tennis players, cyclists, industrial and other professionals who need to kneel and squat for long hours or require repeated stairs and slope negotiation. Exact aetiology of chondromalacia patellae is poorly understood. During knee movement kneecap glides smoothly over the groove of the thigh bone. Which is ensured by the balancing act of different stabilizing factors like thigh muscle, patellar tendon, ligaments, limb alignment and relative contour between knee cap and thigh bone groove. Any deviation of these can cause rubbing or grinding of the knee cap over the thigh bone groove instead of gliding. Abnormal rubbing and grinding of the knee cap causes damage to its cartilage and development of chondromalacia patellae. Following factors can hamper smooth gliding of knee cap over thigh bone:
Most common symptom is dull aching pain in front of the knee underneath the kneecap during squatting, getting up from sitting position, going up and down stairs, going uphill and downhill. While asking to identify location of pain patients cover the entire front of the knee. This can aggravate with stiffness after prolonged sitting like watching a movie in theatre, travelling long in a car or plane. Sometimes the knee can get swell-up with accumulation of knee fluid. A cracking sound or grinding sensation can be felt while moving the knee joint. However having this does not always mean chondromalacia patellae. On examination patellofemoral tenderness is very much evident and can be evoked by different manoeuvres.
Knee x-ray in three plane A/P, lateral and skyline view is the standard basic requirement. In early cases x-ray is non-conclusive. It can detect secondary bony changes in advance cases. Skyline view plays a key role to assess patellofemoral joint alignment. Only MRI can diagnose early cases of chondromalacia patellae. MRI and arthroscopy are the gold standard for diagnosis and assess the severity of cartilage changes in chondromalacia patellae which is described by grading. MRI is non-invasive whereas arthroscopy is invasive and logistically unacceptable only for diagnosis purposes.
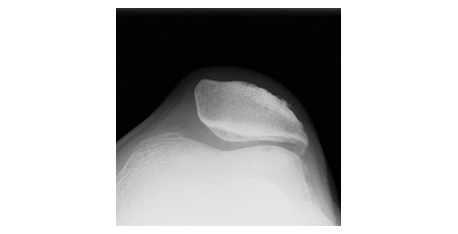
X-Ray showing patellar malalignment
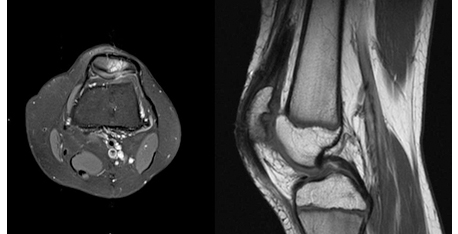
MRI showing Signal changes and other finding at kneecap Cartilage

Arthroscopic view of Kneecap cartilage showing damaged cartilage
Treatment of Chondromalacia patellae is difficult as no single mode of treatment is a full proof method to ensure desirable outcome. Physical therapy is the mainstay of treatment regime. It helps is symptom relieve by offloading knee cap by improving knee muscle strength and gait. Analgesic and icing is helpful in acute condition and recommended for short duration. Commonly practised medical and semi-interventional treatments are,
All of these are being practiced widely with good results. But the outcome is not uniform and sometimes unpredictable. These treatments are effective in early stages of disease only. Surgical treatments are indicated in advance stage of disease and for non-responder to medical management. Different surgical treatments are recommended and practised,
Patellofemoral instability
See in Patellofemoral instability
Quadriceps Tendinopathy
Quadriceps tendinopathy is a painful condition of the knee presented by activity related anterior knee pain with localised tenderness at the upper pole of knee cap and muscle tendon area. It is a degenerative condition of the tendon caused by repeated microtrauma of the tendon due to overuse and other related factors.
Quadriceps tendon is the tendinous attachment of anterior thigh muscle with the upper pole of knee cap. It is the part of extensor mechanism of knee which helps in knee extension, bears body weight and stability of knee joint at different stage of mobilisation. Athletes involving repeated jumping and kneeling activity like basketball and volleyball are at higher risk. Non athletic individuals with high BMI can also develop quadriceps tendinopathy. Hypothyroidism and history of quinolones antibiotic like ciprofloxacin are also considered as risk factor for developing quadriceps tendinopathy.
Symptoms and clinical examination are the keystone of diagnosis. X-ray revels calcification within tendon and irregular bone formation at upper pole of knee cap. USG and MRI both can detect the condition very effectively. Comparing MRI, USG is cost effective.
Conservative treatment with analgesic, icing, activity modification, proper warm-up and physical therapy is the initial mode of treatment. Physiotherapy in the form of stretching of quadriceps muscle, strengthening of hip and back of the knee muscle is effective way of reducing stress and strain on quadriceps muscle and let it heal. Infiltration of affected tendon with PRP helps in its early healing and recovery and indicated for non-responder of conservative management and high end professional athletes. USG guided infiltration increases the accuracy of infiltration and thus better result. Surgical treatment are reserved for very late stage of disease with significant degeneration and tear of tendon. It includes debridement of degenerated tendon with its repair or reconstruction.
Osgood-Schlatter Disease
It is a common painful condition of knee in adolescent, presented by a painful bony bump at anterior aspect of shin bone just below the knee joint where patellar tendon attached. The area is called tibial tuberosity. It happens in children specially who participates in sports activities during their growth spurt. In boys between 12 to14 years and in girls between 10 to 13 years. Intense pain is the early symptom which can aggravate with activity and direct impact. After symptom onset it takes weeks to months to resolve. It usually affects on side but in 20-30% cases it can be bilateral. The condition resolved automatically with the cessation of growth spurt without any residual impact. Very rarely it can be complicated with epiphyseal injury presented as tibial tuberosity avulsion and proximal tibial epiphyseal fracture.
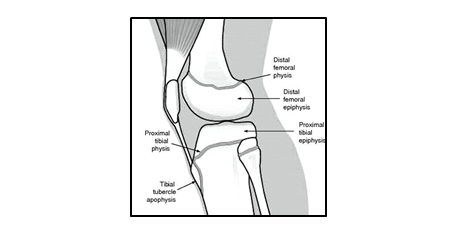
Proximal tibial growth cartilage and Tibial tubercle apophysis
Bone of children and adolescent have a special area of cartilage which allows it to grow and attachment for muscle tendon. The later one is called apophysis. Tibial tubercle is a apophysis of patellar tendon. During growth spurt all the bone, cartilage, muscle and tendon passes through a rapid changes to accommodate the growth. Repeated strong pull of patellar tendon on its attachment at the tibial tubercle apophysis due to sports activity causes alteration of the cartilage architecture and hampers normal growth and fragmentation of the cartilage. Diagnosis is purely clinical. X-ray although not mandatory, can revel fragmentation and fluffiness of apophysis.

X-ray showing fragmentation of tibial tubercle apophysis
Rest, icing, analgesic, modification and restriction of sports activity along with stretching and strengthening exercise improves the symptom. It is a self-limiting condition and healed with very minimal residual changes. Sometimes a asymptomatic prominent tibial tuberosity may remain for life long.

Prominent tibial tubercle of an adult who suffered Osgood-Schlatter disease

Technique of quadriceps stretching in standingBody should not bend or twist while stretching
Jumper's knee or Patellar Tendon Tendinitis
Painful condition of anterior knee with tenderness at inferior pole of knee cap where patellar tendon attached with it. It happens due to repeated microtrauma of patellar tendon due to overstress and lack of recovery time between each trauma. Commonly affects the athlete involved in jumping like volleyball, basketball, high jump and long jump. It can affect non jumping sports like weight lifting, cycling, skiing. Common symptom is pain at the starting of activity may get ease off with continuation of sports during initial stage of disease. But as disease progress it affects the performance. In very advance stage disruption of extensor mechanism can happen. Diagnosis is clinically based, x-ray is indicated to exclude other condition affecting the area. May show calcification at lower pole of knee cap bone or within the tendon in advance stage. USG and MRI both are equally effective in detecting the condition. Treatment consideration is rest, modification of activity, stretching and strengthening of thigh muscle, analgesic and icing. In non-resolving condition USG guided infiltration of PRP is an effective treatment option. In very advanced stage where there is disruption of extensor mechanism or all the non-invasive treatments are exhausted then surgical debridement of the affected tendon with repair is recommended. This can be done both open or arthroscopically.
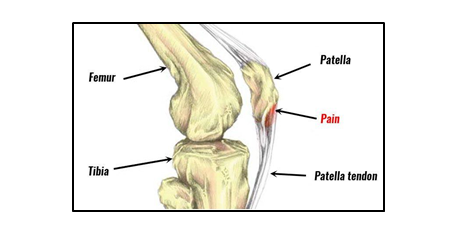
Jumper's knee area of pathology
Hoffa's syndrome
This is also known as infrapatellar fat pad syndrome. It affects the fat pad situated below knee cap. This fat is situated outside the joint but between patellar tendon and joint. It acts as a shock absorber during different arch of knee movement. Commonly the posterolateral part of the fat pad gets impinge between knee cap and thigh bone when knee gets hyper extension, direct blow to anterior part of knee, altered movement due to any fibrosis of fat pad or other injury of the knee. The pain and tenderness usually felt at either side of the patellar tendon. There may be some swelling around it. Pain starts following prolong standing and hyperextension of the knee. Commonly seen in young women participating in jumping sports. Ligamentous laxity causing knee hyperextension is known to be a risk factor. MRI plays a key role in diagnosing the condition and exclusion of other cause of pain. Treatment includes rest, modification of activity, analgesic and icing. Local infiltration of steroid improves the symptom. Although it recovers but may take longer to improve. Rarely surgery is indicated for this condition.
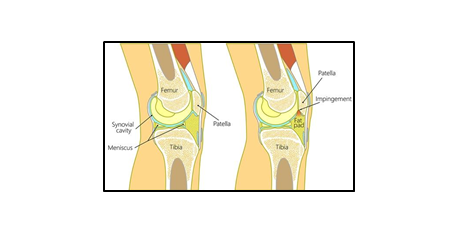
Infra patellar fat pad in normal knee and in Hoffa's syndrome
Iliotibial Band Syndrome
It is a chronic overuse injury of the iliotibial band presented by pain and tenderness at lateral aspect of knee joint at the level of knee cap. It is often associated with weakness of hip abductor muscles. Overuse injury happens due to repeated flexion and extension of knee joint in cyclist and runner. Iliotibial band is a thick fibrous band on lateral aspect of thigh extend from waist bone crossing hip joint to lower leg bone just below knee joint. Area of iliotibial band at the level of most prominent part of lower end of thigh bone is the impingement zone. Impingement happens at 300 of knee flexion when heel strikes the ground and push off during running, the stance phase. Iliotibial band remains in maximum taught situation at this point and knee also gets a varus thrust due to bodies centre of gravity.
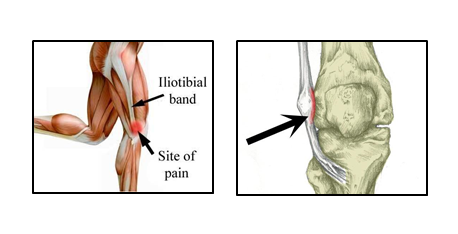
Iliotibial band attachment at waist bone and lower leg bone and area of impingement for IT band syndrome
Pain is the sole symptom of IT band syndrome, which is activity related. Diagnosis is made from the history and local examination. Examination of hip and knee movement, spine deformity, pelvic tilt and knee deformity are assessed to identify any pre-existing risk factor. X-ray and MRI is done mainly to exclude other causes of anterolateral knee pain. MRI can also detect signal changes of IT bands around the impingement zone. Treatment for acute stage is rest, activity modification, analgesic and icing. Physical rehabilitation in the form of IT band starching, posture correction, strengthening of hip, knee and core muscle playas key role. Local infiltration with steroids and PRP can give symptomatic improvement. No surgical intervention is required for this condition.